Breadcrumb
- Home
- Illnesses & Conditions
- Dementia
- Dementia
Content Map Terms
Illnesses & Conditions Categories
-
Allergies
- Allergy to Natural Rubber (Latex)
- Jellyfish Stings: Allergic Reaction
- Allergies: Should I Take Allergy Shots?
- Non-Allergic Rhinitis
- Allergic Reaction
- Allergies
- Allergy Shots for Allergic Rhinitis
- Allergies: Rush Immunotherapy
- Over-the-Counter Medicines for Allergies
- Allergic Rhinitis
- Allergic Rhinitis: Common Triggers
- Allergies: Avoiding Indoor Triggers
- Allergies: Avoiding Outdoor Triggers
- Controlling Dust, Dust Mites, and Other Allergens in Your Home
- Controlling Pet Allergens
- Allergies to Insect Stings
- Allergies: Should I Take Shots for Insect Sting Allergies?
- Immunotherapy for Allergies to Insect Stings
- Types of Allergic Rhinitis
- Allergic Reaction to Tattoo Dye
- Drug Allergies
- Penicillin Allergy
- Hay Fever and Other Seasonal Allergies
- Allergies: Giving Yourself an Epinephrine Shot
-
Arthritis and Osteoporosis
- Rheumatoid Arthritis: Finger and Hand Surgeries
- Rheumatoid Arthritis: Classification Criteria
- Rheumatoid Arthritis: Systemic Symptoms
- Comparing Rheumatoid Arthritis and Osteoarthritis
- Rheumatoid Arthritis: Neck Symptoms
- Osteoporosis in Men
- Psoriatic Arthritis
- Arthritis: Shots for Knee Pain
- Complementary Medicine for Arthritis
- Steve's Story: Coping With Arthritis
- Bev's Story: Coping With Arthritis
- Quick Tips: Modifying Your Home and Work Area When You Have Arthritis
- Coping With Osteoarthritis
- Arthritis: Should I Have Shoulder Replacement Surgery?
- Juvenile Idiopathic Arthritis: Stretching and Strengthening Exercises
- Juvenile Idiopathic Arthritis
- Capsaicin for Osteoarthritis
- Small Joint Surgery for Osteoarthritis
- Osteoarthritis: Heat and Cold Therapy
- Modifying Activities for Osteoarthritis
- Osteoarthritis
- Gout
- Rheumatoid Arthritis
- Juvenile Idiopathic Arthritis: Inflammatory Eye Disease
- Juvenile Idiopathic Arthritis: Range-of-Motion Exercises
- Juvenile Idiopathic Arthritis: Deciding About Total Joint Replacement
- Complications of Osteoarthritis
- Arthritis: Managing Rheumatoid Arthritis
- Arthritis: Should I Have Knee Replacement Surgery?
- Arthritis: Should I Have Hip Replacement Surgery?
- Juvenile Idiopathic Arthritis: Pain Management
- Osteoporosis Risk in Younger Women
- Osteoporosis Screening
-
Asthma
- Asthma: Peak Expiratory Flow and Personal Best
- Asthma and Wheezing
- Asthma: Using an Asthma Action Plan
- Asthma: Measuring Peak Flow
- Asthma: Identifying Your Triggers
- Steroid Medicine for Asthma: Myths and Facts
- Asthma
- Inhaled corticosteroids for asthma
- Inhaled quick-relief medicines for asthma
- Classification of Asthma
- Challenge Tests for Asthma
- Asthma's Impact on Your Child's Life
- Asthma Action Plan: Yellow Zone
- Asthma Triggers
- Asthma Action Plan: Red Zone
- Asthma and GERD
- Occupational Asthma
- Asthma Attack
- Asthma: Symptoms of Difficulty Breathing
- Exercise-Induced Asthma
- Asthma Treatment Goals
- Asthma: Overcoming Obstacles to Taking Medicines
- Asthma in Older Adults: Managing Treatment
- Asthma: Controlling Cockroaches
- Asthma: Educating Yourself and Your Child
- Allergy Shots for Asthma
- Asthma: Taking Charge of Your Asthma
- Monitoring Asthma Treatment
- Omalizumab for Asthma
- Asthma: Ways to Take Inhaled Medicines
- Asthma: Overuse of Quick-Relief Medicines
- Asthma Diary
- Asthma Diary Template
- Asthma Action Plan
- Assessing Your Asthma Knowledge
- My Asthma Action Plan
-
Bowel and Gastrointestinal Conditions
- Abdominal Fullness or Bloating
- Irritable Bowel Syndrome: Criteria for Diagnosis
- Gastritis
- Gas, Bloating, and Burping
- Irritable Bowel Syndrome (IBS)
- Constipation: Keeping Your Bowels Healthy
- Rectal Problems
- Mild, Moderate, or Severe Diarrhea
- Torn or Detached Nail
- Chronic Constipation
- Gas (Flatus)
- Dyspepsia
- Diverticulosis
- Bowel Obstruction
- Anal Fissure
- Bowel Disease: Caring for Your Ostomy
- Anal Fistulas and Crohn's Disease
-
Cancer
- Lung Cancer and Other Lung Problems From Smoking
- Skin Cancer, Non-Melanoma
- Radiation Therapy for Non-Melanoma Skin Cancer
- Colorectal Cancer Test Recommendations
- Breast Cancer Screening: When Should I Start Having Mammograms?
- Lifestyle Changes That May Help Prevent Cancer
- Choosing a Prosthesis After Breast Cancer Surgery
- Hormone Treatment for Breast Cancer
- Cancer Staging and Grading
- Pancreatic Cancer
- Kidney (Renal Cell) Cancer
- Cancer Support: Managing Stress
- Cancer Support: When Your Cancer Comes Back or Gets Worse
- Cancer Support: Dealing With Emotions and Fears
- Cancer Support: Finding Out That You Have Cancer
- Cancer Support: Being an Active Patient
- Cancer Support: Coping With Cancer Treatments
- Cancer Support: Life After Treatment
- Cancer Support: Family, Friends, and Relationships
- Reducing Cancer Risk When You Are BRCA-Positive
- Anal Cancer
- Prostate Cancer: Should I Choose Active Surveillance?
- Lung Cancer Screening
- Basal Cell Skin Cancer: Should I Have Surgery or Use Medicated Cream?
- Tumour Markers
- Does Aspirin Prevent Cancer?
- Cancer
- Lung Cancer
- Oral Cancer
- Colorectal Cancer
- Metastatic Melanoma
- Radiation Treatment for Cancer
- Skin Cancer, Melanoma
- Cervical Cancer Screening
- Hepatitis B and C: Risk of Liver Cancer
- Inflammatory Bowel Disease (IBD) and Cancer Risk
- Radiation Therapy for Prostate Cancer
- Prostate Cancer
- Cancer: Home Treatment for Mouth Sores
- Skin Cancer Screening
- Breast Cancer: Should I Have Breast Reconstruction After a Mastectomy?
- Prostate Cancer: Should I Have Radiation or Surgery for Localized Prostate Cancer?
- Prostate Cancer Screening
- Side Effects of Chemotherapy
- Breast Cancer: Lymph Node Surgery for Staging Cancer
- Endometrial (Uterine) Cancer
- Cryosurgery for Prostate Cancer
- Breast Cancer
- Cancer: Home Treatment for Nausea or Vomiting
- Cancer: Home Treatment for Pain
- Cancer: Home Treatment for Diarrhea
- Cancer: Home Treatment for Constipation
- Breast Cancer Types
- Cancer: Home Treatment for Sleep Problems
- Cancer: Home Treatment for Fatigue
- Hair Loss From Cancer Treatment
- Body Image After Cancer Treatment
- Breast Cancer: Should I Have Breast-Conserving Surgery or a Mastectomy for Early-Stage Cancer?
- Breast Cancer, Metastatic or Recurrent
- Cancer Pain
- Leukemia
- Colorectal Cancer, Metastatic or Recurrent
- Thyroid Cancer
- Types of Thyroid Cancer
- Radiation Therapy for Cancer Pain
- Breast Cancer in Men (Male Breast Cancer)
- Breast Cancer Screening
- Breast Cancer: Should I Have Chemotherapy for Early-Stage Breast Cancer?
- Asbestos and Lung Cancer
- Cervical Cancer
- Ovarian Cancer
- Colorectal Cancer Genetic Testing
- Testicular Cancer Screening
- Skin Cancer: Protecting Your Skin
- Non-Melanoma Skin Cancer: Comparing Treatments
- Bladder Cancer
- Prostate Cancer, Advanced or Metastatic
- Active Surveillance for Prostate Cancer
- Urinary Problems and Prostate Cancer
- Cancer: Controlling Cancer Pain
- Heat and Cold Treatment for Cancer Pain
- Testicular Cancer
- Testicular Cancer: Which Treatment Should I Have for Stage I Non-Seminoma Testicular Cancer After My Surgery?
- Testicular Cancer: Which Treatment Should I Have for Stage I Seminoma Testicular Cancer After My Surgery?
- Cancer: Controlling Nausea and Vomiting From Chemotherapy
- Lymphedema: Managing Lymphedema
- Breast Cancer Risk: Should I Have a BRCA Gene Test?
- Inflammatory Breast Cancer
- Ovarian Cancer: Should I Have My Ovaries Removed to Prevent Ovarian Cancer?
- Family History and the Risk for Breast or Ovarian Cancer
- Breast Cancer: What Should I Do if I'm at High Risk?
-
Cold and Flu
- Difference Between Influenza (Flu) and a Cold
- Colds and Flu
- Influenza (Flu) Complications
- Common Questions About the Influenza (Flu) Vaccine
- Influenza (Seasonal Flu)
- Whooping Cough (Pertussis)
- Productive Coughs
- Dry Coughs
- Influenza (Flu): Should I Take Antiviral Medicine?
- Flu Vaccines: Should I Get a Flu Vaccine?
- Relieving A Cough
- Colds
-
COPD
- Cal's Story: Learning to Exercise When You have COPD
- Conserving Energy When You Have COPD or Other Chronic Conditions
- Nebulizer for COPD Treatment
- COPD Action Plan
- COPD: Help for Caregivers
- COPD: Keeping Your Diet Healthy
- COPD: Using Exercise to Feel Better
- COPD
- COPD Flare-Ups
- Bullectomy for COPD
- COPD and Alpha-1 Antitrypsin (AAT) Deficiency
- COPD and Sex
- Pulmonary Rehabilitation
- COPD
- Oxygen Treatment for Chronic Obstructive Pulmonary Disease (COPD)
- COPD: Avoiding Weight Loss
- COPD: Avoiding Your Triggers
-
Dementia
- Alzheimer's or Other Dementia: Should I Move My Relative Into Long-Term Care?
- Alzheimer's and Other Dementias: Coping With Sundowning
- Dementia: Assessing Pain
- Medical History and Physical Examination for Dementia or Alzheimer's Disease
- Alzheimer's and Other Dementias: Making the Most of Remaining Abilities
- Dementia: Helping a Person Avoid Confusion
- Alzheimer's and Other Dementias: Maintaining Good Nutrition
- Dementia: Tips for Communicating
- Agitation and Dementia
- Dementia: Bladder and Bowel Problems
- Dementia: Support for Caregivers
- Dementia: Legal Issues
- Dementia: Understanding Behaviour Changes
- Dementia: Medicines to Treat Behaviour Changes
- Dementia
- Mild Cognitive Impairment and Dementia
-
Diabetes
- Diabetes: Blood Sugar Levels
- Diabetes: Counting Carbs if You Don't Use Insulin
- Diabetes: Coping With Your Feelings About Your Diet
- Diabetes: Tracking My Feelings
- Diabetes: Taking Care of Your Feet
- Diabetes: Care of Blood Sugar Test Supplies
- Diabetes: Checking Your Blood Sugar
- Diabetes: Checking Your Feet
- Diabetes: Steps for Foot-Washing
- Diabetes: Protecting Your Feet
- Diabetes: Dealing With Low Blood Sugar From Medicines
- Diabetes: Dealing With Low Blood Sugar From Insulin or Medicine
- Diabetes: How to Give Glucagon
- Low Blood Sugar Level Record
- Symptoms of Low Blood Sugar
- Diabetes: Preventing High Blood Sugar Emergencies
- Diabetic Ketoacidosis (DKA)
- High Blood Sugar Level Record
- Symptoms of High Blood Sugar
- Diabetes: Using Canada's Food Guide
- Diabetes: Giving Yourself an Insulin Shot
- Glycemic Index
- Diabetes and Alcohol
- Continuous Glucose Monitoring
- Quick Tips: Diabetes and Shift Work
- Diabetes: How to Prepare for a Colonoscopy
- Type 2 Diabetes: Can You Cure It?
- Diabetes, Type 2: Should I Take Insulin?
- Prediabetes: Which Treatment Should I Use to Prevent Type 2 Diabetes?
- Diabetes: Making Medical Decisions as Your Health Changes
- Diabetes Care Plan
- Diabetes: Caregiving for an Older Adult
- Quick Tips: Smart Snacking When You Have Diabetes
- Testing Tips From a Diabetes Educator
- Gloria's Story: Adding Activity to Help Control Blood Sugar
- Andy's Story: Finding Your Own Routine When You Have Diabetes
- Jerry's Story: Take Prediabetes Seriously
- Linda's Story: Getting Active When You Have Prediabetes
- Diabetes
- Tips for Exercising Safely When You Have Diabetes
- Diabetes: Travel Tips
- Type 2 Diabetes
- Type 1 Diabetes
- Care of Your Skin When You Have Diabetes
- Diabetes: Taking Care of Your Teeth and Gums
- Non-insulin medicines for type 2 diabetes
- Metformin for diabetes
- Hypoglycemia (Low Blood Sugar) in People Without Diabetes
- Diabetic Retinopathy
- Laser Photocoagulation for Diabetic Retinopathy
- Diabetic Neuropathy
- Diabetic Atypical Neuropathies
- Diabetic Neuropathy: Exercising Safely
- Diabetic Autonomic Neuropathy
- Criteria for Diagnosing Diabetes
- Diabetes-Related High and Low Blood Sugar Levels
- Diabetic Nephropathy
- Diabetes: Counting Carbs if You Use Insulin
- Diabetes: Cholesterol Levels
- Diabetes and Infections
- Diabetes: Tests to Watch for Complications
- Diabetes: Differences Between Type 1 and 2
- Diabetes Complications
- How Diabetes Causes Blindness
- How Diabetes Causes Foot Problems
- Reading Food Labels When You Have Diabetes
- Eating Out When You Have Diabetes
- Breastfeeding When You Have Diabetes
- Diabetes: Staying Motivated
- Sick-Day Guidelines for People With Diabetes
- Diabetes: Amputation for Foot Problems
- Prediabetes
- Prediabetes: Exercise Tips
- Type 2 Diabetes: Screening for Adults
- Diabetes: Should I Get an Insulin Pump?
- Diabetes: Living With an Insulin Pump
- Form for Carbohydrate Counting
-
Disease and Disease Prevention
- Diseases and Conditions
- Osgood-Schlatter Disease
- Needle Aponeurotomy for Dupuytren's Disease
- Mitochondrial Diseases
- Disease and Injury Prevention
- Alzheimer's Disease
- Root Planing and Scaling for Gum Disease
- Kawasaki Disease
- Tay-Sachs Disease
- Von Willebrand's Disease
- Hirschsprung's Disease
- Complications of Paget's Disease
- Paget's Disease of Bone
- Celiac Disease
- Peptic Ulcer Disease
- Ménière's Disease
- Pelvic Inflammatory Disease: Tubo-Ovarian Abscess
- Pelvic Inflammatory Disease
- Addison's Disease
- Misdiagnosis of Lyme Disease
- Lyme Disease
- Parkinson's Disease and Freezing
- Parkinson's Disease: Other Symptoms
- Parkinson's Disease: Modifying Your Activities and Your Home
- Parkinson's Disease and Tremors
- Parkinson's Disease and Speech Problems
- Parkinson's Disease
- Disease-modifying antirheumatic drugs (DMARDs)
- Parkinson's Disease: Movement Problems From Levodopa
- Mad Cow Disease
- Handwashing
- Peyronie's Disease
- Stages of Lyme Disease
- Osteotomy and Paget's Disease
- Dupuytren's Disease
- Crohn's Disease
- Crohn's Disease: Problems Outside the Digestive Tract
- Pilonidal Disease
- Acquired Von Willebrand's Disease
-
Down Syndrome, Autism and Developmental Delays
- Autism
- Down Syndrome: Helping Your Child Eat Independently
- Down Syndrome: Grooming and Hygiene
- Down Syndrome: Helping Your Child Learn to Walk and Use Other Motor Skills
- Down Syndrome: Helping Your Child Learn to Communicate
- Down Syndrome
- Dyslexia
- Conditions Related to Dyslexia
- Autism: Behavioural Training and Management
- Autism: Support and Training for the Family
- Unproven Treatments for Autism
- Caring for Adults With Autism
- Down Syndrome: Helping Your Child Avoid Social Problems
- Down Syndrome: Training and Therapy for Young People
- Down Syndrome: Helping Your Child Dress Independently
- Down Syndrome, Ages Birth to 1 Month
- Down Syndrome, Ages 1 Month to 1 Year
- Down Syndrome, Ages 1 to 5
- Down Syndrome, Ages 5 to 13
- Down Syndrome, Ages 13 to 21
- Eating Disorders
-
Epilepsy
- Absence Epilepsy
- Juvenile Myoclonic Epilepsy
- Temporal Lobe Epilepsy
- Focal Epilepsy
- Epilepsy: Focal Aware Seizures
- Epilepsy
- Epilepsy and Driving
- Epilepsy: Generalized Seizures
- Epilepsy: Generalized Tonic-Clonic Seizures
- Epilepsy: Myoclonic Seizures
- Epilepsy: Atonic Seizures
- Epilepsy: Tonic Seizures
- Epilepsy: Focal Impaired Awareness Seizures
- Epilepsy Medicine Therapy Failure
- Stopping Medicine for Epilepsy
- Questions About Medicines for Epilepsy
- Epilepsy: Taking Your Medicines Properly
-
Fatigue and Sleep
- Sleep Apnea: Should I Have a Sleep Study?
- Sleep and Your Health
- Quick Tips: Making the Best of Shift Work
- Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Managing Your Energy
- Sleeping Better
- Sleep Problems
- Doxepin (Sleep) - Oral
- Improving Sleep When You Have Chronic Pain
- Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
- Chronic Fatigue: Changing Your Schedule
- Chronic Fatigue: Getting Support
- Snoring and Obstructive Sleep Apnea
- Coping With Changing Sleep Patterns as You Get Older
- Stages of Sleep
- Sleep Apnea: Fibre-Optic Pharyngoscopy
- Oral Breathing Devices for Sleep Apnea and Snoring
- Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea
- Sleep Apnea
- Sleep Problems, Age 12 and Older
- Stages of Sleep Apnea
- Sleep Journal
- Shift Work Sleep Disorder
- Snoring
- Sleep Problems: Dealing With Jet Lag
- Insomnia
- Sleep and Your Body Clock
- Weakness and Fatigue
- Insomnia: Improving Your Sleep
-
Heart Health and Stroke
- Peripheral Arterial Disease
- Bradycardia (Slow Heart Rate)
- Types of Bradycardia
- Cardiac Device Monitoring
- Angioplasty for Peripheral Arterial Disease of the Legs
- Isolated Systolic High Blood Pressure
- Atrial Fibrillation: Should I Try Electrical Cardioversion?
- Change in Heartbeat
- Deep Vein Thrombosis
- Fast Heart Rate
- Heart Failure: Symptom Record
- Heart Failure: Compensation by the Heart and Body
- Heart Failure: Taking Medicines Properly
- Heart Failure: Watching Your Fluids
- Heart Failure: Avoiding Triggers for Sudden Heart Failure
- Heart Failure: Activity and Exercise
- Heart Tests: When Do You Need Them?
- Low Blood Pressure (Hypotension)
- Cardiac Arrest
- Heart Failure Daily Action Plan
- Premature Ventricular Contractions (PVCs)
- Heart Rate Problems: Should I Get a Pacemaker?
- Heart Rhythm Problems: Should I Get an Implantable Cardioverter-Defibrillator (ICD)?
- What to Do if Your Cardiac Device Is Recalled
- Venous Insufficiency
- Carotid Artery Stenting
- ICD: Living Well With It
- Diabetes: Lower Your Risk for Heart Attack and Stroke
- Pacemaker for Heart Failure (Cardiac Resynchronization Therapy)
- Heart Attack: How to Prevent Another One
- Stroke: How to Prevent Another One
- Sex and Your Heart
- Supraventricular Tachycardia: Should I Have Catheter Ablation?
- Carotid Artery Disease
- Giant Cell Arteritis
- High Blood Pressure: Over-the-Counter Medicines to Avoid
- Postural Orthostatic Tachycardia Syndrome (POTS)
- Leg Aneurysm
- Pulmonary Hypertension
- Left Ventricular Hypertrophy (LVH)
- Heart Failure: Checking Your Weight
- Alan's Story: Coping With Change After a Heart Attack
- Coronary Artery Disease: Prevention Myths
- Quick Tips: Taking Charge of Your Angina
- Heart and Circulation
- High Blood Pressure
- Heartburn
- Angioplasty for Coronary Artery Disease
- Coronary Artery Disease
- Implantable Cardioverter-Defibrillator (ICD)
- Aortic Valve Regurgitation
- Aortic Valve Stenosis
- Secondary High Blood Pressure
- Hemorrhagic Stroke
- Stroke: Common Problems
- Self-Care After a Stroke
- Stroke: Dealing With Depression
- Stroke: Getting Dressed
- Stroke: Speech and Language Problems
- Stroke: Bladder and Bowel Problems
- Stroke: Preventing Injury in Affected Limbs
- After a Stroke: Helping Your Family Adjust
- Stroke: Behaviour Changes
- Stroke: Changes in Emotions
- Stroke: Perception Changes
- Stroke: Problems With Ignoring the Affected Side
- Stroke: Memory Tips
- Stroke: Your Rehabilitation Team
- Stroke
- Transient Ischemic Attack (TIA)
- Cardiac Rehabilitation: Lifestyle Changes
- Cardiac Rehabilitation: Hospital Program
- Cardiac Rehabilitation: Home Program
- Cardiac Rehabilitation: Outpatient Program
- Cardiac Rehabilitation: Maintenance Program
- Congenital Heart Defects
- Congenital Heart Disease: Caring for Your Child
- Coronary Artery Disease: Should I Have an Angiogram?
- Sudden Heart Failure
- Classification of Heart Failure
- Heart Failure: Tips for Easier Breathing
- Heart Failure: Avoiding Colds and Flu
- Heart Failure
- Helping Someone During a Panic Attack
- Aortic Aneurysm
- High Blood Pressure
- Coronary Artery Disease: Family History
- Angina
- Using Nitroglycerin for Angina
- Heartburn: Changing Your Eating Habits
- Angiotensin II receptor blockers (ARBs)
- Beta-blockers
- Heart Rhythm Problems: Diary of Symptoms
- Vagal Manoeuvres for Supraventricular Tachycardia (SVT)
- Electrical Cardioversion (Defibrillation) for a Fast Heart Rate
- Catheter Ablation for a Fast Heart Rate
- Supraventricular Tachycardia
- Home Blood Pressure Log
- Blood Pressure Screening
- Heart Block
- Electrical System of the Heart
- Heart Rhythm Problems and Driving
- Heart Rhythm Problems: Symptoms
- Resuming Sexual Activity After a Heart Attack
- Risk Factors for Coronary Artery Disease
- Pacemaker for Bradycardia
- SPECT Image of the Heart
- Heart Attack and Stroke in Women: Reducing Your Risk
- Ventricular Tachycardia
- Aspirin to Prevent Heart Attack and Stroke
- Temporal Artery Biopsy
- Emergency First Aid for Heatstroke
- Heartburn Symptom Record
- Heart Attack and Unstable Angina
- Congenital Heart Disease in Adults
- Monitoring and Medicines for Heart Failure
- Ventricular Assist Device (VAD) for Heart Failure
- Cardiac Output
- Heart Failure Symptoms
- Heart Failure: Less Common Symptoms
- Heart Failure With Reduced Ejection Fraction (Systolic Heart Failure)
- Heart Failure With Preserved Ejection Fraction (Diastolic Heart Failure)
- High-Output Heart Failure
- Right-Sided Heart Failure
- Heart Failure Complications
- How the Heart Works
- Coronary Arteries and Heart Function
- Heart Failure Types
- Enjoying Life When You Have Heart Failure
- Heart Failure: Tips for Caregivers
- Medicines to Prevent Abnormal Heart Rhythm in Heart Failure
- Cardiac Cachexia
- Heart Failure Stages
- Cardiac Rehabilitation Team
- Cardiac Rehabilitation: Emotional Health Benefits
- Ischemia
- Coronary Artery Disease: Roles of Different Doctors
- Coronary Artery Disease: Helping a Loved One
- Manage Stress for Your Heart
- Intermittent Claudication
- Peripheral Arterial Disease: Pulse and Blood Pressure Measurement
- Heart Failure and Sexual Activity
- Joan's Story: Coping With Depression and Anxiety From Heart Failure
- Rheumatic Fever and the Heart
- Heart Valve Problems: Should I Choose a Mechanical Valve or Tissue Valve to Replace My Heart Valve?
- Acute Coronary Syndrome
- Aspirin: Should I Take Daily Aspirin to Prevent a Heart Attack or Stroke?
- Heart Failure: Should I Get a Pacemaker ?
- Heart Failure: Should I Get an Implantable Cardioverter-Defibrillator (ICD)?
- Heart Valve Disease
- Myxoma Tumours of the Heart
- Aortic Dissection
- Heart Attack and Stroke Risk Screening
- High Blood Pressure: Checking Your Blood Pressure at Home
- Hypertensive Emergency
- Stroke Rehabilitation
- Treatment for Stroke-Related Spasticity
- Driving a Car After a Stroke
- Heart Failure: Avoiding Medicines That Make Symptoms Worse
- Stroke Recovery: Coping With Eating Problems
- Heart Murmur
- High Blood Pressure: Should I Take Medicine?
- Coronary Artery Disease: Should I Have Angioplasty for Stable Angina?
- Tyrell's Story: Taking Pills for High Blood Pressure
- Stroke Prevention: Should I Have a Carotid Artery Procedure?
- Atrial Fibrillation: Which Anticoagulant Should I Take to Prevent Stroke?
- Stroke: Should I Move My Loved One Into Long-Term Care?
- Atrial Fibrillation: Should I Take an Anticoagulant to Prevent Stroke?
- Smoking and Coronary Artery Disease
-
Hepatitis
- Hepatitis C: Your Risk for Cirrhosis
- Hepatitis E
- Hepatitis B Immune Globulin - Injection
- Heparin - Injection
- Fulminant Hepatitis
- Protect Yourself From Hepatitis A When Travelling
- Hepatitis A
- Viral Hepatitis
- Hepatitis C
- Hepatitis D
- Hepatitis B: How to Avoid Spreading the Virus
- Hepatitis B
- Hepatitis Panel
- Hepatitis B Treatment Recommendations
- Hepatitis B: Should I Be Tested?
-
HIV
- HIV Infection
- HIV Viral Load
- HIV: Stages of Infection
- Ways HIV Cannot Be Spread
- HIV and Exercise
- HIV: Giving Support
- HIV: Tips for Caregivers to Avoid Infection
- HIV: Preventing Other Infections When You Have HIV
- HIV Home Care
- Antiretroviral medicines for HIV
- Resistance to HIV Medicines
- HIV: Preventing Infections
- HIV: Antiretroviral Therapy (ART)
- Opportunistic Infections in HIV
- HIV: Taking Antiretroviral Medicines
- HIV: Non-Progressors and HIV-Resistant People
- HIV Screening
- HIV and Weight Loss
- HIV and Fatigue
-
Infectious Diseases
- Anthrax
- Avian Influenza
- Avoiding Infections in the Hospital
- Bacterial Infections of the Spine
- Bites and Stings: Flu-Like Symptoms
- Boric Acid for Vaginal Yeast Infection
- Caregiving: Reducing Germs and Infection in the Home
- Central Vascular Access Device (CVAD): Flushing
- Chickenpox (Varicella)
- Chickenpox: Preventing Skin Infections
- Chikungunya Fever
- Complicated Urinary Tract Infections
- Complications of Ear Infections
- Cranberry Juice and Urinary Tract Infections
- Dengue Fever
- Ear Infection: Should I Give My Child Antibiotics?
- Ear Infections
- Ebola or Marburg Virus Infection
- Ebola Virus Disease
- Enterovirus D68 (EV-D68)
- Fever or Chills, Age 11 and Younger
- Fever or Chills, Age 12 and Older
- Fever Seizures
- Feverfew for Migraines
- Fifth Disease
- Flu: Signs of Bacterial Infection
- Fungal Nail Infections
- Giardiasis
- Hand-Foot-and-Mouth Disease
- Kissing Bugs
- Measles (Rubeola)
- Middle East Respiratory Syndrome (MERS)
- Molluscum Contagiosum
- Monkeypox
- Mononucleosis (Mono)
- Mononucleosis Complications
- Mumps
- Nail Infection: Should I Take Antifungal Pills?
- Neutropenia: Preventing Infections
- Non-Surgical Nail Removal for Fungal Nail Infections
- Noroviruses
- Pleurisy
- Pneumonia
- Preventing Tetanus Infections
- Pseudomonas Infection
- Recurrent Ear Infections and Persistent Effusion
- Recurrent Vaginal Yeast Infections
- Respiratory Syncytial Virus (RSV) Infection
- Rotavirus
- Rubella (German Measles)
- Scarlet Fever
- Sexually Transmitted Infections
- Sexually Transmitted Infections: Genital Examination for Men
- Sexually Transmitted Infections: Symptoms in Women
- Sexually Transmitted Infections: Treatment
- Shingles
- Smallpox
- Sore Throat and Other Throat Problems
- Staph Infection
- Strep Throat
- Symptoms of Pelvic Infection
- Thrush
- Tick Bites: Flu-Like Symptoms
- Tinea Versicolor
- Tuberculosis (TB)
- Tuberculosis (TB) Screening
- Urinary Tract Infections (UTIs): Risks for Older Adults
- Vaginal Yeast Infection: Should I Treat It Myself?
- Vaginal Yeast Infections
- Valley Fever
- West Nile Virus
- Zika Virus
- Informed Health Decisions
-
Injuries
- Trapped Finger, Toe, or Limb
- Blister Care
- Exercises for Heel Pain or Tightness
- Broken Toe
- Broken Nose (Nasal Fracture)
- Preventing Blisters
- Hip Fracture
- Medial Collateral Ligament (MCL) Injury
- Pressure Injuries From Scuba Diving
- Pressure Injuries: Stages
- Pressure Injuries: Prevention and Treatment
- Calf Muscle Injury
- Avulsion Fracture
- Lateral Collateral Ligament (LCL) Injury
- Posterior Cruciate Ligament (PCL) Injury
- Frozen or Stuck Tongue or Other Body Part
- Jones Fracture
- Animal and Human Bites
- Blisters
- Burns and Electric Shock
- Choking Rescue Procedure: Heimlich Manoeuvre
- Cold Temperature Exposure
- Cuts
- Ear Problems and Injuries, Age 11 and Younger
- Elbow Injuries
- Elbow Problems, Non-Injury
- Facial Injuries
- Facial Problems, Non-Injury
- Fish Hook Injuries
- Toe, Foot, and Ankle Injuries
- Groin Problems and Injuries
- Finger, Hand, and Wrist Injuries
- Anterior Cruciate Ligament (ACL) Injuries
- Safe Hand and Wrist Movements
- Physical Rehabilitation for ACL Injuries
- Marine Stings and Scrapes
- Mouth Problems, Non-Injury
- Nail Problems and Injuries
- Puncture Wounds
- Shoulder Problems and Injuries
- Removing Splinters
- Swallowed Button Disc Battery, Magnet, or Object With Lead
- Object Stuck in the Throat
- How a Scrape Heals
- Removing an Object From a Wound
- Types of Chest Injuries
- Injury to the Tailbone (Coccyx)
- First Aid for a Spinal Injury
- Body Mechanics
- Scrapes
- Swallowed or Inhaled Objects
- Swelling
- Overuse Injuries
- Meniscus Tear
- Razor Bumps
- Ankle Sprain
- Sprained Ankle: Using a Compression Wrap
- High-Pressure Injection Wounds
- Patellar Dislocation
- Hamstring Muscles
- Plica in the Knee
- Spondylolysis and Spondylolisthesis
- Pressure Injuries
- Heat After an Injury
- Concussion
- Navicular (Scaphoid) Fracture of the Wrist
- Cold Exposure: What Increases Your Risk of Injury?
- Broken Collarbone
- Shoulder Separation
- Frozen Shoulder
- Preventing ACL Injuries
- Living With a Spinal Cord Injury
- Classification of Spinal Cord Injuries
- Tendon Injury (Tendinopathy)
- Shin Splints
- Muscle Cramps
- Whiplash
- Broken Rib
-
Joints and Spinal Conditions
- Osteochondritis Dissecans of a Joint
- Returning to Work With Low Back Pain
- Moving From Sitting to Standing
- Golfer's Elbow
- Bones, Joints, and Muscles
- Hip Injuries, Age 11 and Younger
- Hip Injuries, Age 12 and Older
- Hip Problems, Age 12 and Older
- Rotator Cuff Disorders
- Osteoporosis
- Spina Bifida
- Temporomandibular Disorders: Having Good Body Mechanics
- Temporomandibular Disorders (TMD)
- Tennis Elbow
- Debridement for Rotator Cuff Disorders
- Spinal Curves in Scoliosis
- Spondyloarthropathies
- Knee Problems and Injuries
- Posture: Standing and Walking
- Osteoporosis Risk Factors
- Bruxism and Temporomandibular Disorders
- Patellar Subluxation
- Steroid-Induced Osteoporosis
- Cervical Spinal Stenosis
- Lumbar Spinal Stenosis
- Spasticity
- Scoliosis In Adults
- Acute Flaccid Myelitis
- Spinal Cord Injury: Abdominal Thrust Assist (Assisted Cough)
- Spinal Cord Injury: Your Rehabilitation Team
- Spinal Cord Injury: Talking With Your Partner About Sex
- Mobility After a Spinal Cord Injury
- Spinal Cord Injury: Adapting Your Home
- Spinal Cord Injury: Safe Transfers To or From a Wheelchair
- Spinal Cord Injury: Autonomic Dysreflexia
- Back Problems and Injuries
- Proper Sitting for a Healthy Back
- Brace (Orthotic) Treatment for Scoliosis
- Proper Back Posture (Neutral Spine)
- Severity of Back Injuries
- Back Problems: Proper Lifting
- Degenerative Disc Disease
-
Kidneys
- Acute Kidney Injury Versus Chronic Kidney Disease
- Nephrotic Syndrome
- Uremia
- Kidney Stones: Should I Have Lithotripsy to Break Up the Stone?
- Chronic Kidney Disease
- Kidney Failure: When Should I Start Dialysis?
- Kidney Failure: Should I Start Dialysis?
- Anemia of Chronic Kidney Disease
- End-Stage Kidney Failure
- Tolvaptan (Inherited Kidney Disease) - Oral
- Types of Kidney Stones
- Extracorporeal Shock Wave Lithotripsy (ESWL) for Kidney Stones
- Percutaneous Nephrolithotomy or Nephrolithotripsy for Kidney Stones
- Kidney Stones
- Advance Care Planning: Should I Stop Kidney Dialysis?
- Chronic Kidney Disease: Medicines to Be Careful With
- Stages of Chronic Kidney Disease
- Medicines That Can Cause Acute Kidney Injury
- Donating a Kidney
- Kidney Stones: Medicines That Increase Your Risk
-
Lung and Respiratory Conditions
- Breathing Problems: Using a Metered-Dose Inhaler
- Acute Respiratory Distress Syndrome (ARDS)
- Bronchiectasis
- Chest Problems
- Sildenafil 20 Mg (Lungs) - Oral
- Tadalafil (Lungs) - Oral
- Tests for Lung Infections
- COPD: Lung Volume Reduction Surgery
- Acute Bronchitis
- Respiratory Problems, Age 11 and Younger
- Respiratory Problems, Age 12 and Older
- Breathing Smoke or Fumes
- Pulmonary (Lung) Nodules
- Severe Acute Respiratory Syndrome (SARS)
- COPD's Effect on the Lungs
- Black Lung Disease
- Oral Breathing Devices for Snoring
- Spinal Cord Injury: Breathing Practice
- Breathing Problems: Using a Dry Powder Inhaler
- COPD: Clearing Your Lungs
- Collapsed Lung (Pneumothorax)
- Interactive Tool: Should I Consider Surgery for My Low Back Problem?
- Lung Problems: Learning to Breathe Easier
- Lung Function in COPD
- COPD: Handling a Flare-Up
- Sarah's Story: Dealing With the Emotions From COPD
- Fran's Story: Finding Support When You Have COPD
-
Multiple Sclerosis
- Multiple Sclerosis: Alternative Treatments
- Multiple Sclerosis: Modifying Your Home
- Multiple Sclerosis: Bladder Problems
- Multiple Sclerosis (MS)
- Types of Multiple Sclerosis
- Multiple Sclerosis Progression
- Multiple Sclerosis: MRI Results
- Multiple Sclerosis: Mental and Emotional Problems
- Multiple Sclerosis: Questions About What to Expect
- Rehabilitation Programs for Multiple Sclerosis
- Obesity
-
Rehabilitation and Exercise
- Breathing Exercises: Using a Manual Incentive Spirometer
- Sensual Exercises for Erection Problems
- Breastfeeding: Exercise and Weight Loss
- Jaw Problems: Exercise and Relaxation
- Exercises for Arm and Wrist
- Kegel Exercises
- Tennis Elbow: Stretches and Strengthening Exercises
- Cardiac Rehabilitation: Exercise
- Neck Exercises
- Stress Management: Imagery Exercises
- Sprained Ankle: Rehabilitation Exercises
- Plantar Fasciitis: Exercises to Relieve Pain
- Cardiac Rehabilitation: Medicine and Exercise
- Cardiac Rehabilitation: Monitoring Your Body's Response to Exercise
- Rotator Cuff Problems: Exercises You Can Do at Home
- Stress Management: Breathing Exercises
- ACL Injury: Exercises to Do Before Treatment
- Spinal Cord Injury: Sensual Exercises
- Martha's Story: A Voice for Recovery
- Stan's Story: Getting There Hasn't Been Easy
- Debbie's Story: People Can and Do Recover
- Susan's Story: A Friend Really Helps
- Meniscus Tear: Rehabilitation Exercises
- Patellar Tracking Disorder: Exercises
- Stress Management: Breathing Exercises for Relaxation
- Good-Health Attitude
-
Sexual, Reproductive Health
- Menopause: Should I Use Hormone Therapy (HT)?
- Abnormal Uterine Bleeding: Should I Have a Hysterectomy?
- PMS: Should I Try an SSRI Medicine for My Symptoms?
- Sexual Orientation
- Gender Identity Issues: Getting Support
- Heavy Menstrual Periods
- Pubic Lice
- Menopause and Your Risk for Other Health Concerns
- Menstrual Cups
- Gender Dysphoria
- Menstrual Cramps: Relieving Pain
- Men's Health
- Sexual and Reproductive Organs
- Sexual Health
- Women's Health
- Genital Warts
- Sexuality While Breastfeeding
- Premenstrual Syndrome (PMS)
- Chlamydia
- Sexuality and Physical Changes With Aging
- Relieving Menstrual Pain
- Uterine Fibroids
- Gonorrhea
- Syphilis
- Neurosyphilis
- Congenital Syphilis
- Emotions and Menopause
- Hot Flashes and Menopause
- Vaginal Dryness
- Genital Herpes
- Parkinson's Disease and Sexual Problems
- Male Genital Problems and Injuries
- Menstrual Cramps
- Missed or Irregular Periods
- Genital Self-Examination
- Missed Periods and Endurance Training
- Rashes or Sores in the Groin
- Other Health Problems Caused by Herpes Simplex Virus
- Arrhythmias and Sexual Activity
- Stages of Syphilis
- Normal Vaginal Discharge
- Vaginal Rashes and Sores
- Vaginal Fistula
- Soy for Menopause Symptoms
- Menopause: Wild Yam and Progesterone Creams
- Normal Menstrual Cycle
- Vaginal Pessaries
- Uterine Fibroid Embolization (UFE)
- Uterine Fibroids: Should I Use GnRH-A Therapy?
- Uterine Fibroids: Should I Have Uterine Fibroid Embolization?
- Menopause: Managing Hot Flashes
- Premature Ejaculation
- High-Risk Sexual Behaviour
- Object in the Vagina
- Periodic Limb Movement Disorder
- Military Sexual Trauma
- Sexual Problems in Women
- Female Genital Problems and Injuries
- Smoking: Sexual and Reproductive Problems
-
Skin, Nails and Rashes
- Hidradenitis Suppurativa
- Removing Moles and Skin Tags
- Caregiving: Skin Care for Immobile Adults
- Yeast Skin Infection
- Bruises and Blood Spots Under the Skin
- Skin, Hair, and Nails
- Nail Psoriasis
- Phototherapy for Psoriasis
- Psoriasis
- Ringworm of the Skin
- Rash, Age 12 and Older
- Sunburn: Skin Types
- Heat Rash
- Colour Changes in Nails
- Changes in Your Nails
- Cut That Removes All Layers of Skin
- Skin Changes
- Venous Skin Ulcer
- Venous Skin Ulcers: Home Treatment
- Eczema: Taking Care of Your Skin
- Seborrheic Keratoses
- Care for a Skin Wound
- Psoriasis: Skin, Scalp, and Nail Care
- Protecting Your Skin From the Sun
- Skin Rashes: Home Treatment
- Skin Cyst: Home Treatment
- Calluses and Corns
- Calluses and Corns: Using Pumice Stones
- Calluses and Corns: Protective Padding
- Tazarotene (Psoriasis/Acne) - Topical
- Types of Acne
- Acne: Treatment With Benzoyl Peroxide
- Acne: Treatment With Alpha Hydroxy Acids
- Acne: Treatment With Salicylic Acid
- Acne: Treatment With Antibiotics
- Acne
- Acne: Tips for Keeping It Under Control
- Acne: Should I Take Isotretinoin for Severe Acne?
- Acne: Should I See My Doctor?
-
Thyroid
- Hyperthyroidism: Should I Use Antithyroid Medicine or Radioactive Iodine?
- Thyroid Storm
- Hyperparathyroidism
- Thyroid - Oral
- Subclinical Hypothyroidism
- Hypothyroidism
- Hyperthyroidism: Graves' Ophthalmopathy
- Radioactive Iodine for Hyperthyroidism
- Hyperthyroidism
- Thyroid Nodules
- Thyroid Hormone Production and Function
- Vertigo
- Check Your Symptoms
- Search Health Topics
British Columbia Specific Information
In British Columbia, people with dementia and their families have access to information and support to make informed choices about their long-term care. First Link® is an early intervention service designed to connect individuals and families affected by Alzheimer's disease or another dementia with services and support as soon as possible after diagnosis. For more information on First Link® visit Alzheimer Society – FirstLink® form referrals.
The Ministry of Health, in collaboration with physicians and nurses from across B.C., has developed the Best Practice Guideline for Accommodating and Managing Behavioural and Psychological Symptoms of Dementia in Residential Care. The guideline includes a useful algorithm and is intended to support health care providers when they provide care and support to people with Alzheimer’s or other dementia and their families.
If you or a loved one are having difficulty coping with activities of daily living because of a health-related problem such as dementia, A Guide to Your Care (PDF 1.66 MB) may help you. The guide has information about home and community care services to help British Columbians live as independently as possible. For additional information on home and community care services in B.C. including care options and cost, who pays for care, eligibility requirements, and how to arrange care, visit the Home & Community Care website.
For more information about health care service delivery, visit The Alzheimer Society's Guidelines for Care: Person-Centred Care of People with Dementia Living in Care Homes Framework (PDF 526 KB), or the British Columbia Psychogeriatric Association's resource Meeting Seniors' Mental Health Care Needs in British Columbia: A Resource Document (PDF 1.66 MB).
Condition Basics
What is dementia?
We all forget things as we get older. Many older people have a slight loss of memory that does not affect their daily lives. But memory loss that gets worse may mean that you have dementia.
Dementia is a loss of mental skills that affects your daily life. It can cause problems with memory, problem-solving, and learning. It also can cause problems with thinking and planning.
Dementia usually gets worse over time. But how quickly it gets worse is different for each person. Some people stay the same for years. Others lose skills quickly.
Your chances of having dementia rise as you get older. But this doesn't mean that everyone will get it.
What causes it?
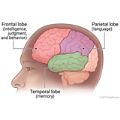
Dementia is caused by damage to or changes in the brain. Alzheimer's disease is the most common cause. Strokes are the second most common cause. Other causes include diseases such as Parkinson's disease and frontotemporal dementia.
What are the symptoms?
Usually the first symptom of dementia is memory loss. Often the person with memory loss doesn't notice it. As dementia gets worse, the person may have trouble doing things that take planning. He or she may have trouble using or understanding words or may get lost in well-known places.
How is it diagnosed?
There is no single test for dementia. To diagnose dementia, your doctor will do a physical examination and ask questions about illnesses and life events. Your doctor may test your memory by asking you to tell what day and year it is, repeat a series of words, or draw a clock face.
How is dementia treated?
Medicines for dementia can make it easier to live with. They may help improve mental function, mood, or behaviour. An active social life, counselling, and sometimes medicine may help with changing emotions.
How can you care for someone who has dementia?
Care needs will change over time. You'll work with health professionals to create a safe and comfortable environment and make tasks of daily living easier. You can help by making sure the person eats well. You can also help manage sleep problems. Your loved one may also need help with bladder and bowel control.
Cause
Dementia is caused by damage to or changes in the brain. Things that can cause dementia include:
- Alzheimer's disease. This is the most common cause.
- Strokes, tumours, or head injuries. This type of dementia is called vascular dementia.
- Diseases. These include Parkinson's disease, dementia with Lewy bodies, and frontotemporal dementia.
Some disorders that cause dementia can run in families. Doctors often suspect an inherited cause if someone younger than 50 has symptoms of dementia.
Learn more
Symptoms
Usually the first symptom of dementia is memory loss. Often the person who has the memory problem doesn't notice it, but family and friends do.
People who have dementia may have increasing trouble with:
- Recalling recent events. They may forget appointments or lose objects.
- Recognizing people and places.
- Keeping up with conversations and activity.
- Finding their way around familiar places, or driving to and from places they know well.
- Keeping up personal care such as grooming or bathing.
- Planning and carrying out routine tasks. They may have trouble following a recipe or writing a letter or email.
What Happens
How quickly dementia progresses depends on what is causing it and the area of the brain that is affected. Some types of dementia progress slowly over several years. Other types may progress more quickly.
The course of dementia varies greatly from one person to another. An early diagnosis and treatment with medicines may help for a while. Even without these medicines, some people remain stable for months or years, while others get worse quickly.
Many people with dementia aren't aware of their mental decline.
Over time, depending on the type of dementia, the way the person behaves may change. The person may become angry or agitated, or clingy and childlike. They may wander and become lost.
Even with the best care, people who have dementia tend to have a shorter lifespan than the average person their age.
When to Call a Doctor
Call 9-1-1 or other emergency services immediately if signs of a stroke or transient ischemic attack (TIA) develop suddenly. These may include:
- Numbness, weakness, or inability to move the face, arm, or leg, especially on one side of the body.
- Vision problems in one or both eyes, such as dimness, blurring, double vision, loss of vision, or feeling like a shade is being pulled down over your eyes.
- Confusion, or trouble speaking or understanding.
- Trouble walking, dizziness, or loss of balance or coordination.
- Severe headache with no known cause.
Call a doctor now if a person suddenly becomes confused or emotionally upset or doesn't seem to know who or where they are. These are signs of delirium, which can be caused by a reaction to medicines or a new or worsening medical condition.
Call a doctor if you or a person you are close to has new and troubling memory loss that is more than an occasional bout of forgetfulness. This may be an early sign of dementia.
Watchful waiting
Occasional forgetfulness or memory loss can be a normal part of aging. But any new or increasing memory loss or problems with daily living should be reported to a doctor. Learn the warning signs of dementia, and talk to a doctor if you or a family member shows any of these signs. They include increased trouble finding the right words when speaking, getting lost going to familiar places, and acting more irritable or suspicious than usual.
Examinations and Tests
To diagnose dementia, your doctor will:
- Do a physical examination.
- Ask questions about recent and past illnesses and life events. The doctor will want to talk to a close family member to check details.
- Ask you to do some simple things that test your memory and other mental skills. Your doctor may ask you to tell what day and year it is, repeat a series of words, or draw a clock face.
The doctor may do tests to look for a cause that can be treated. For example, you might have blood tests to check your thyroid or to look for an infection. You might also have a test that shows a picture of your brain, like an MRI or a CT scan. These tests can help your doctor find a tumour or brain injury.
Knowing the type of dementia a person has can help the doctor prescribe medicines or other treatments.
Learn more
Treatment Overview
Medicines for dementia can slow it down for a while and make it easier to live with. Medicines can't cure it. But they may help improve mental function, mood, or behaviour.
If a stroke caused the dementia, doing things to reduce the chance of another stroke may help. They include eating healthy foods, being active, staying at a healthy weight, and not smoking.
As dementia gets worse, a person may get depressed or angry and upset. An active social life, counselling, and sometimes medicine may help with changing emotions.
The goals of ongoing treatment are to keep the person safely at home as long as possible and to provide support and guidance to the caregivers.
The person will need routine follow-up visits. The doctor will monitor medicines and the person's level of functioning.
Self-Care
- Take your medicines exactly as prescribed. Call your doctor or nurse advice line if you think you are having a problem with your medicine.
- Eat healthy foods. Eat lots of whole grains, fruits, and vegetables every day. If you are not hungry, try snacks or nutritional drinks such as Boost or Ensure.
- If you have problems sleeping:
- Try not to nap too close to your bedtime.
- Exercise regularly. Walking is a good choice.
- Try a glass of warm milk or caffeine-free herbal tea before bed.
- Do tasks and activities during the time of day when you feel your best. It may help to develop a daily routine.
- Post labels, lists, and sticky notes to help you remember things. Write your activities on a calendar you can easily find. Put your clock where you can easily see it.
- Stay active. Take walks in familiar places, or with friends or loved ones. Try to stay active mentally too. Read and work crossword puzzles if you enjoy these activities.
- Do not drive unless you can pass an on-road driving test. If you are not sure if you are safe to drive, your provincial ministry of transportation can test you.
- Keep a cordless phone and a flashlight with new batteries by your bed. If possible, put a phone in each of the main rooms of your house, or carry a cell phone in case you fall and cannot reach a phone. Or, you can wear a device around your neck or wrist. You push a button that sends a signal for help.
Acknowledge your emotions and plan for the future
- Talk openly and honestly with your doctor.
- Let yourself grieve. It is common to feel angry, scared, frustrated, anxious, or depressed.
- Get emotional support from family, friends, a support group, or a counsellor experienced in working with people who have dementia.
- Ask for help if you need it.
- Tell your doctor how you feel. You may feel upset, angry, or worried at times. Many things can cause this, including poor sleep, medicine side effects, confusion, and pain. Your doctor may be able to help you.
- Plan for the future.
- Talk to your family and doctor about preparing an advance care plan and other important papers while you can make decisions. These papers tell your doctors how to care for you at the end of your life.
- Consider naming a person to make decisions about your care if you are not able to.
Medicines
Doctors use medicines to treat dementia by:
- Maintaining mental function for as long as possible.
- Managing mood or behaviour problems. These include depression, insomnia, hallucinations, and agitation.
- Preventing more strokes in people who have dementia caused by stroke (vascular dementia).
Medicines to help maintain mental function
These medicines may include:
- Cholinesterase inhibitors. Examples are donepezil and galantamine.
- Memantine.
Medicines to help control mood or behaviour problems
Many behaviour problems can be managed without medicines.
In some cases, the doctor may prescribe:
- Antidepressants. Examples are citalopram and trazodone.
- Antipsychotic drugs. Examples are olanzapine and risperidone.
Medicines to prevent future strokes
The doctor may prescribe medicines for high blood pressure and high cholesterol. These drugs can't reverse existing dementia. But they may prevent future strokes and heart disease that can lead to more brain damage.
Learn more
Caring for Someone Who Has Dementia
Taking care of the person
- If the person takes medicine for dementia, help him or her take it exactly as prescribed. Call your doctor or nurse advice line if you notice any problems with the medicine.
- Make a list of the person's medicines. Review it with all of his or her doctors.
- Help the person eat a balanced diet. Serve plenty of whole grains, fruits, and vegetables every day. If the person is not hungry at mealtimes, give snacks at midmorning and in the afternoon. Offer drinks such as Boost or Ensure if the person is losing weight.
- Encourage exercise. Walking and other activities may slow the decline of mental ability. Help the person stay active mentally with reading, crossword puzzles, or other hobbies.
- Talk openly with the doctor about any behaviour changes. Many people who have dementia become easily upset or agitated or feel worried. There are many things that can cause this, such as medicine side effects, confusion, and pain. It may be helpful to:
- Keep distractions to a minimum. It may also help to keep noise levels low and voices quiet.
- Develop simple daily routines for bathing, dressing, and other activities. And remind your loved one often about upcoming changes to the daily routine, such as trips or appointments.
- Ask what is upsetting him or her. Keep in mind that people who have dementia don't always know why they are upset.
- Take steps to help if the person is sundowning. This is the restless behaviour and trouble with sleeping that may occur in late afternoon and at night. Try not to let the person nap during the day. Offer a glass of warm milk or caffeine-free tea before bedtime.
- Be patient. A task may take the person longer than it used to.
- For as long as he or she is able, allow your loved one to make decisions about activities, food, clothing, and other choices. Let him or her be independent, even if tasks take more time or are not done perfectly. Tailor tasks to the person's abilities. For example, if cooking is no longer safe, ask for other help. Your loved one can help set the table, or make simple dishes such as a salad. When the person needs help, offer it gently.
Staying safe
- Make your home (or your loved one's home) safe. Tack down rugs, and put no-slip tape in the tub. Install handrails, and put safety switches on stoves and appliances. Keep rooms free of clutter. Make sure walkways around furniture are clear. Do not move furniture around, because the person may become confused.
- Use locks on doors and cupboards. Lock up knives, scissors, medicines, cleaning supplies, and other dangerous things.
- Do not let the person drive or cook if he or she can't do it safely. A person with dementia should not drive unless he or she is able to pass an on-road driving test. Your provincial ministry of transportation can do a driving test if there is any question.
- Get medical alert jewellery for the person so that you can be contacted if he or she wanders away. If possible, provide a safe place for wandering, such as an enclosed yard or garden.
Taking care of yourself
- Ask your doctor about support groups and other resources in your area.
- Take care of your health. Be sure to eat healthy foods and get enough rest and exercise.
- Take time for yourself. Respite services provide someone to stay with the person for a short time while you get out of the house for a few hours.
- Make time for an activity that you enjoy. Read, listen to music, paint, do crafts, or play an instrument, even if it's only for a few minutes a day.
- Spend time with family, friends, and others in your support system.
Learn more
- Agitation and Dementia
- Alzheimer's and Other Dementias: Coping With Sundowning
- Alzheimer's and Other Dementias: Maintaining Good Nutrition
- Alzheimer's and Other Dementias: Making the Most of Remaining Abilities
- Care at the End of Life
- Caregiver Tips
- Caregiving: Making a Home Safe
- Dementia: Assessing Pain
- Dementia: Support for Caregivers
- Dementia: Tips for Communicating
- Memory Problems: Issues With Driving
- Memory Problems: Tips for Helping the Person With Daily Tasks
- Memory Problems: Wandering
Related Information
Credits
Current as of: October 20, 2022
Author: Healthwise Staff
Medical Review:
Anne C. Poinier MD - Internal Medicine
Kathleen Romito MD - Family Medicine
Myron F. Weiner MD - Psychiatry, Neurology
Current as of: October 20, 2022
Author: Healthwise Staff
Medical Review:Anne C. Poinier MD - Internal Medicine & Kathleen Romito MD - Family Medicine & Myron F. Weiner MD - Psychiatry, Neurology
This information does not replace the advice of a doctor. Healthwise, Incorporated disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated.
Alzheimer Society of British Columbia: First Link Dementia Helpline
The First Link® Dementia Helpline is for anyone affected by dementia, whether professionally or personally. If you have questions about Alzheimer's disease or other dementias, call the Alzheimer Society of B.C.'s First Link® Dementia Helpline for information and support (toll-free):
- English: 1-800-936-6033 (Monday to Friday, 9 a.m. to 8 p.m.)
- Cantonese and Mandarin: 1-833-674-5007 (Monday to Friday, 9 a.m. to 4 p.m.)
- Punjabi: 1-833-674-5003 (Monday to Friday, 9 a.m. to 4 p.m.)
For more information on First Link® visit: