Condition Basics
What is gastroesophageal reflux disease?
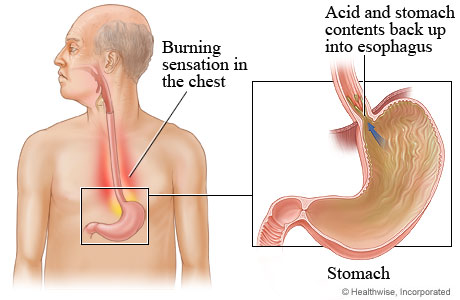
Reflux means that stomach acid and juices flow from the stomach back up into the esophagus, the tube that connects the throat to the stomach. This causes heartburn. When you have heartburn that bothers you often, it is called gastroesophageal reflux disease, or GERD. This can also cause pain and swelling in your esophagus (esophagitis).
Eating too much late at night or before lying down sometimes can cause heartburn and a sour taste in the mouth. But having heartburn from time to time doesn't mean that you have GERD. With GERD, the reflux and heartburn last longer and happen more often.
What causes it?
Normally when you swallow food, it travels down the esophagus. A valve opens to let the food pass into the stomach, and then the valve closes. With GERD, the valve doesn't close tightly enough. Stomach acid and juices from the stomach flow back up (reflux) into the esophagus.
What are the symptoms of GERD?
The main symptom of GERD is ongoing heartburn. It may feel like a burning, warmth, or pain just behind the breastbone. You may also have a sour or bitter taste in your mouth. It is common to have symptoms at night when you're trying to sleep.
How is it diagnosed?
Your doctor may ask about your symptoms, such as whether you often have heartburn. If you do, your doctor may recommend a medicine that reduces or blocks stomach acid. If your heartburn goes away after you take the medicine, your doctor will probably diagnose GERD.
How is GERD treated?
Treatment starts with changing your habits and taking over-the-counter medicines. For example, eating several small meals a day instead of three large ones may help. Try medicines such as antacids (like Tums) or H2 blockers (like Pepcid). If symptoms persist, a doctor may suggest more testing, a change in medicine, or surgery.
What can you do to reduce your symptoms?
Take your medicines as directed. These may include prescription or over-the-counter medicines. Eat several small meals a day. Avoid foods that make your GERD worse, like chocolate, mint, and spicy foods. After eating, wait 2 to 3 hours before lying down. For night-time symptoms, raise the head of your bed 15 to 20 centimetres.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
GERD happens because of a problem with the ring of muscle at the end of the esophagus called the lower esophageal sphincter. It acts like a one-way valve between the esophagus and the stomach. When you swallow, the valve lets food pass into the stomach. With GERD, the valve doesn't close tightly enough. Stomach acid and juices flow back up (reflux) into the esophagus.
GERD usually happens when the valve relaxes at the wrong time and stays open too long. Some things may relax the valve so it doesn't close tightly or some foods and drinks can make GERD worse. These may include chocolate, mint, alcohol, pepper, spicy foods, high-fat foods, or drinks with caffeine in them, such as tea, coffee, colas, or energy drinks. If your symptoms are worse after you eat a certain food, you may want to stop eating it to see if your symptoms get better.
Other things can make stomach juices back up, such as:
- Hormonal changes during pregnancy.
- A weak lower esophageal sphincter.
- A hiatal hernia.
- Slow digestion.
- An overfull stomach.
What Increases Your Risk
Things that increase your risk for symptoms of gastroesophageal reflux disease (GERD) include your lifestyle and certain health conditions.
Lifestyle
- Being overweight.
- Smoking.
- Eating certain foods. These may include chocolate, mint, alcohol, pepper, spicy foods, high-fat foods, or drinks with caffeine in them, such as tea, coffee, colas, or energy drinks. If your symptoms are worse after you eat a certain food, you may want to stop eating it to see if your symptoms get better.
Health conditions
- Being pregnant. GERD is a common problem during pregnancy. Most of the time, symptoms get better after the baby is born.
- Having a hiatal hernia.
- Taking certain medicines. If you think that a medicine you take may be causing your GERD symptoms, talk to your doctor.
Learn more
- Gastroesophageal Reflux Disease (GERD) During Pregnancy
- Hiatal Hernia
Prevention
You may be able to prevent GERD with lifestyle changes, such as eating a healthy diet, not smoking, and staying at a healthy weight.
Some medicines may cause GERD as a side effect. If any medicines you take seem to be the cause of your heartburn, talk with your doctor. Don't stop taking a prescription medicine until you talk with your doctor.
Symptoms
The main symptoms of GERD are:
- Ongoing (persistent) heartburn. Heartburn is an uncomfortable feeling or burning pain behind the breastbone. It may occur after you eat, soon after you lie down, or when you bend forward. Some people have GERD without heartburn.
- A sour or bitter taste in the mouth. This is caused by the backflow of stomach acid and juices into the esophagus.
Other symptoms may include:
- Chest pain. If you have pain in your chest, it is important to make sure that it isn't caused by a problem with your heart.
- The pain caused by GERD usually happens after you eat. It may occur with heartburn.
- Pain from the heart usually feels like heaviness, tightness, discomfort, or a dull ache. It occurs most often after you are active.
- Hoarseness.
- Trouble swallowing (more common with advanced GERD).
- A feeling that something is stuck in your throat.
- A cough.
- Having extra saliva.
- Nausea.
What Happens
GERD may cause irritation or inflammation in the esophagus, the tube that connects the throat to the stomach. This condition is called esophagitis.
Mild GERD symptoms are an uncomfortable feeling of burning, warmth, heat, or pain just behind the breastbone. You may be able to treat these symptoms with over-the-counter medicines that reduce or block acid.
Advanced GERD can cause problems such as:
- Severe esophagitis, esophageal erosion, and ulcers.
- A narrowed esophagus.
- Barrett's esophagus. With this, the cells that line the inside of the esophagus are replaced by cells like those that line the inside of the stomach and intestine.
- Respiratory problems. These include a cough that won't go away, asthma, pneumonia, and laryngitis.
- The speeding up of tooth decay. This is because stomach acid gets into the mouth and wears away tooth enamel.
Some people who have GERD may have a higher risk for cancer of the esophagus.
Learn more
When to Call a Doctor
The main symptom of GERD is an uncomfortable feeling of burning, warmth, heat, or pain just behind the breastbone. This feeling is often called heartburn. Sometimes heartburn can feel like the chest pain of a heart attack.
Call 9-1-1 or other emergency services immediately if:
- You have symptoms of a heart attack. These may include:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly or in one or both shoulders or arms.
- Light-headedness or sudden weakness.
- A fast or irregular heartbeat.
After you call 9-1-1, the operator may tell you to chew 1 adult-strength or 2 to 4 low-dose aspirin. Wait for an ambulance. Do not try to drive yourself.
Call your doctor now if you:
- Vomit blood.
- Have bloody, black, or maroon-coloured stools.
Call your doctor if your GERD symptoms:
- Do not improve after 2 weeks of home treatment, are different or are getting worse, or are interfering with normal activities.
- Occur with choking or trouble swallowing.
- Occur with a lot of weight loss when you aren't trying to lose weight.
- Have occurred frequently over several years and are only partly relieved with lifestyle changes and non-prescription medicines that reduce or block acid.
Watchful waiting
Watchful waiting is a wait-and-see approach. If your heartburn is mild and happens only now and then, you may get relief by making lifestyle changes and taking non-prescription medicines that reduce or block acid.
Examinations and Tests
To find out if you have GERD, your doctor will do a physical examination and ask you questions about your health. Your doctor may ask about your symptoms, such as whether you often have heartburn. If you do have heartburn often, your doctor may suggest a medicine that reduces or blocks stomach acid.
If your heartburn goes away after you take the medicine, your doctor will probably diagnose GERD. You may or may not need any tests.
If medicines don't help, you may have tests. These tests may include:
- An upper gastrointestinal endoscopy.
- Esophageal tests.
- An upper-gastrointestinal X-ray series.
Learn more
Treatment Overview
Treatment aims to reduce reflux, prevent damage to your esophagus, and prevent problems caused by GERD.
For mild symptoms, try over-the-counter medicines such as:
- Antacids (like Tums).
- H2 blockers (like famotidine).
- Proton pump inhibitors (like omeprazole).
Lifestyle changes are important. You can:
- Eat several small meals instead of three large meals.
- Wait 2 to 3 hours after eating before lying down.
- Avoid foods that make your symptoms worse. These may include chocolate, mint, alcohol, pepper, spicy foods, high-fat foods, or drinks with caffeine in them, such as tea, coffee, colas, or energy drinks. If your symptoms are worse after you eat a certain food, you may want to stop eating it to see if your symptoms get better.
- Raise the head of your bed 15 to 20 centimetres (6 to 8 inches).
- Lose weight if needed. Losing just 2.5 to 4.5 kilograms (5 to 10 pounds) can help.
If symptoms persist, possible next steps include a change in medicine or testing. Your doctor may recommend surgery to strengthen the valve between your esophagus and stomach.
Learn more
Medicines
Antacids, H2 blockers, and proton pump inhibitors (PPIs) are usually tried first to treat GERD and its symptoms. These can be either prescription or over-the-counter.
Medicines can:
- Relieve symptoms (heartburn, sour taste, or pain).
- Allow the esophagus to heal.
- Prevent problems caused by GERD.
You may take:
- Antacids. These include Gaviscon and Tums. Antacids neutralize stomach acid and relieve heartburn. If you want to take medicine only when your symptoms bother you, antacids are a good choice.
- Acid reducers, such as:
- H2 blockers. These include cimetidine and famotidine (Pepcid). H2 blockers reduce the amount of acid in the stomach. Most are sold in both over-the-counter and prescription strength.
- PPIs. These include lansoprazole (Prevacid) and omeprazole (Losec). PPIs reduce the amount of acid in the stomach. Some are available over-the-counter.
If your daily medicine doesn't control your GERD symptoms, talk with your doctor. You may need to try a different medicine.
Learn more
Surgery
Surgery may be used to treat GERD symptoms that haven't been controlled well by medicines.
The most common surgery used to treat GERD is fundoplication. It strengthens the valve (lower esophageal sphincter) between the esophagus and stomach. This helps keep acid from backing up into the esophagus as easily. It relieves GERD symptoms and inflammation of the esophagus.
It may be done in one of two ways.
- A partial fundoplication. With this, the stomach is wrapped only partway around the esophagus.
- A full fundoplication. With this, the stomach is wrapped all the way around the esophagus.
Gastropexy is another type of surgery for GERD. With this, the stomach is attached to the diaphragm. It is done so that the stomach can't move through the opening in the diaphragm into the chest.
Surgery for GERD can cause problems with swallowing, burping, and extra gas. You may need other procedures to fix these problems.
Learn more
Related Information
Credits
Current as of: March 22, 2023
Author: Healthwise Staff
Medical Review:
Adam Husney MD - Family Medicine
E. Gregory Thompson MD - Internal Medicine
Kathleen Romito MD - Family Medicine
Elizabeth T. Russo MD - Internal Medicine
Arvydas D. Vanagunas MD - Gastroenterology
Current as of: March 22, 2023
Author: Healthwise Staff
Medical Review:Adam Husney MD - Family Medicine & E. Gregory Thompson MD - Internal Medicine & Kathleen Romito MD - Family Medicine & Elizabeth T. Russo MD - Internal Medicine & Arvydas D. Vanagunas MD - Gastroenterology



